A National Surgical Quality Improvement Program (NSQIP) Analysis of Trends in Trainee Participation in Infrainguinal Bypasses and the Effect Upon Intraoperative and Postoperative and Outcomes
Bernardino C. Branco, MD, Miguel Montero-Baker, MD, Ramyar Gilani, MD, Charles A. West, MD, Joseph L. Mills, MD, Jayer Chung, MD, MSc.
Baylor College of Medicine, Houston, TX, USA.
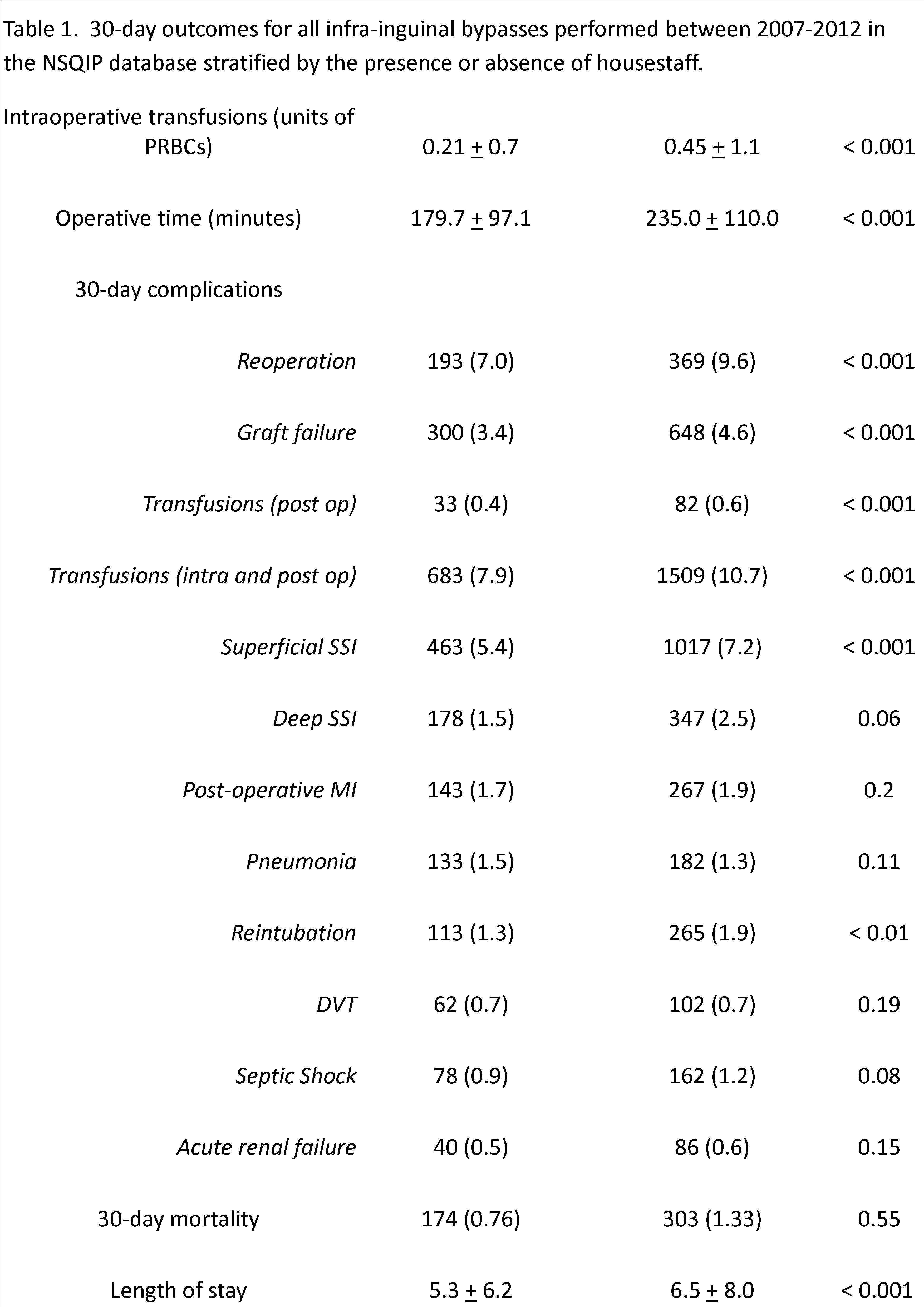
Background: The effect of resident duty hour restrictions and increasing endovascular procedural volumes upon operative proficiency for open vascular surgery remains controversial. Hence, we aimed to determine trends in operative experience and outcomes for infrainguinal bypass (IB) stratified by the presence or absence of trainees. Methods: We evaluated IB’s in the National Surgical Quality Improvement Program (NSQIP) from 2007-2012 stratifying the patients between those operated by an attending-alone (ATT), versus those with an attending and resident (RES). Propensity scores were used to match patients by ATT and RES. Chi-squared, t-tests and Cochrane-Armitage tests were used where appropriate. Results: Over six years, 22,746 patients underwent IB (mean age 68.1 + 11.7 years; 14,503 male [63.8%]), comprising the unmatched cohort. 8,618 (37.9%) IB’s were performed by an attending alone, whereas 14,128 (62.1%) were performed with housestaff. Over the study period, there was a statistically significant increase in the proportion of IB’s performed by ATT (31.0% in 2007 to 45.9% in 2012; p = 0.03). ATT had non-statistically significant lower 30-day mortality, but a statistically significant lower rate of 30-day complications and length of stay (Table 1). After propensity-matching, statistically significant lower lengths of stay (p < 0.001), operative times (p < 0.001), re-operation rates (p = 0.002) and transfusion requirements (intra- and post-operative; p < 0.001) persisted in the ATT arm. Data regarding the specific post-graduate year (PGY) level was available only from 2007-2010. There were non-statistically significant decreases in the proportion of cases performed by fellows (PGY > 6; from 28.8% in 2007 to 22.9% in 2010; p = 0.39) and chief residents (PGY 4 and 5; from 29.2% in 2007 to 26.3% in 2010, p = 0.64). Conclusions: There is a gap in intra-and post-operative outcomes between ATT and RES that results in a statistically significant increase in 30-day morbidity, length of stay, and frequency of re-operation. Given the differences in outcomes, the increasing trend of IB’s performed by attendings-alone represents a critical lost educational opportunity. Further adjustments to training programs are required to optimize IB educational experiences while minimizing patient morbidity and utilization of healthcare resources.
Back to 2017 Program




