Preloaded Catheters and Guide-Wire Systems to Facilitate Catheterization During Fenestrated and Branched Endovascular Aortic Repair
Julia Chini1, Gustavo Oderich, MD1, Mauricio Ribeiro, MD, PhD1, Giuliano Sandri, MD1, Stephen Cha, MS2, Jan Hofer, RN1, Jean Wigham, RN1.
1Mayo Clinic, Rochester, MN, USA, 2Mayo Clinic, Phoenix, AZ, USA.
OBJECTIVES: Pre-loaded systems (PLS) with catheter/ guide-wires allow immediate access to fenestrations and directional branches facilitating fenestrated-branched endovascular aortic repair (F-BEVAR). Limitations include the need for larger profile devices (22Fr) and the risk of vascular trauma or cerebral emboli associated with brachial access. The aim of this study was to review clinical outcomes from patients undergoing F-BEVAR with PLS to treat pararenal (PRA) and thoracoabdominal aortic aneurysms (TAAAs).
METHODS: We reviewed clinical data of 83 patients enrolled in a prospective study to investigate F-BEVAR (NCT 1937949 and NCT2089607). Devices were designed with PLS to access at least two vessels (celiac and SMA) from the brachial approach (Figure). End-points were technical success (defined by placement of the aortic and side stent components), total endovascular and lower extremity ischemia time, 30-day mortality, major adverse events (MAEs), stroke rates, and extremity ischemic complications.
RESULTS: There were 64 male and 19 female patients with a mean age of 75±7 years old. Aneurysm extent was PRA in 27 patients and TAAA in 56. A total of 333 target vessels were incorporated (4±0.4 vessels/patient). Technical success was 99.7%. Total endovascular time was 160±51 minutes and total lower extremity ischemia time was 115±42 minutes. There were no 30-day mortalities. Fifteen patients (18%) had MAEs, including three ischemic strokes. Of these, two patients had minor bilateral strokes in anterior-posterior circulation and one had a major anterior circulation stroke ipsilateral to brachial access. All strokes occurred in female patients (16% vs 0%, P=0.001). There were no upper extremity ischemic or neurologic complications.
CONCLUSIONS: This study shows high technical success and earlier lower limb reperfusion with F-BEVAR using PLS accessed via brachial approach. Stroke, although minor in most patients, remains a concern particularly in female patients. 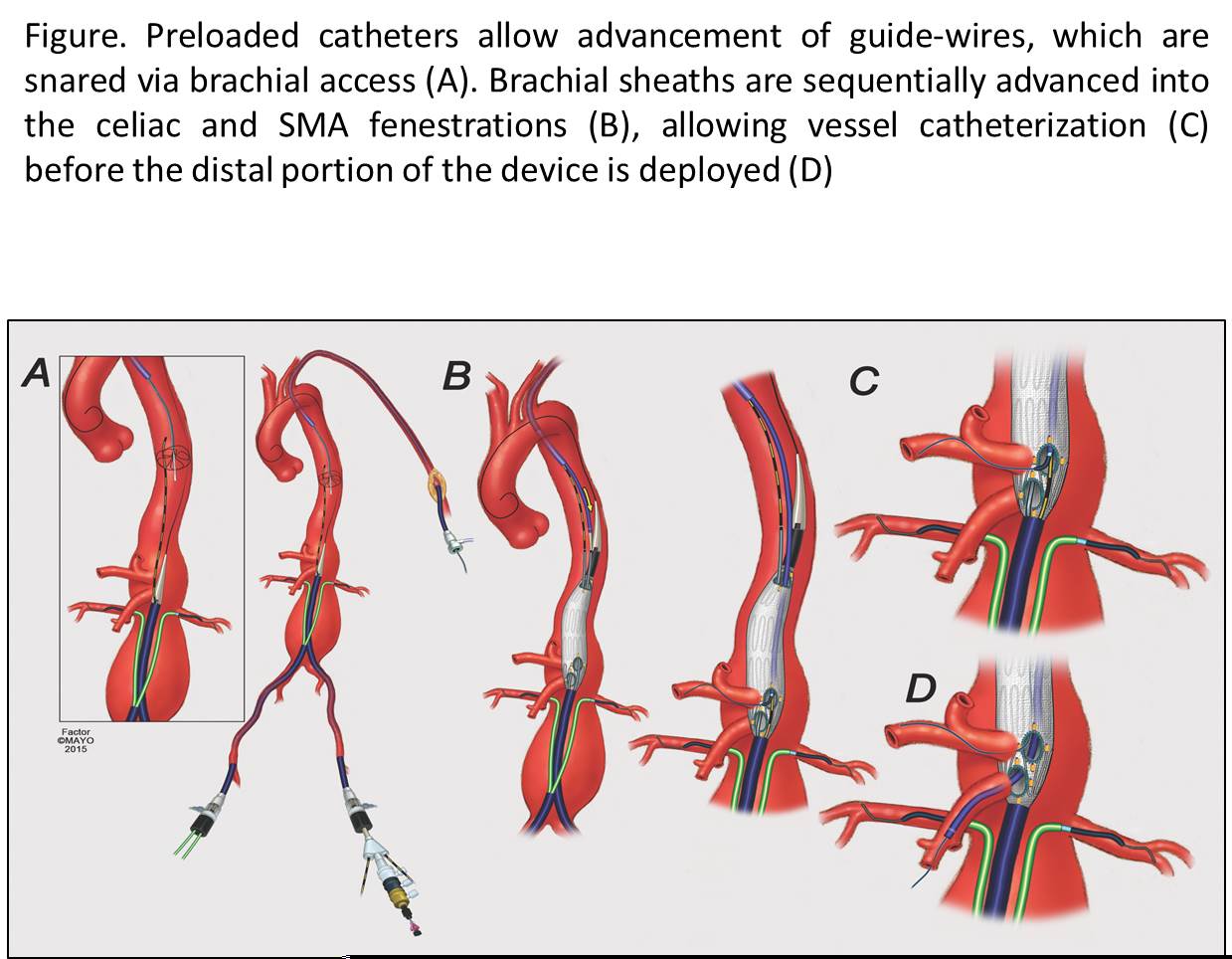
Back to 2017 Program




